Most skin rashes do not harm your health, with redness and itching resolving on their own, even without medications or a visit to a GP. However, you should never ignore a rash, especially when your symptoms worsen or persist for several days.
Our skin is the largest organ in the body. It protects us from the environment, regulates body temperature, excretes waste products, absorbs water, and facilitates sensation. The skin is the window to our overall health. When compromised, we become susceptible to infection, dryness, and irritation, including factors that can cause a skin rash.
This rash guide explains skin rashes, their causes, and when you should see Dr Ritu at our clinic for a rash assessment in our Ultimo clinic.
Common Causes of Rashes
Rashes are a generalised term for skin irritation and can be due to various factors. The following are the most common reasons for developing a rash:
Heat Rash

Heat rash. Source: Raisingchildren.net.au
Heat rash develops when a sweat duct becomes blocked or inflamed, trapping sweat beneath the skin’s surface. This leads to irritation and the hallmark bumps on the skin. Babies are most commonly affected by heat rash (miliaria).
Sometimes, a heat rash may occur deeper in the skin, causing prickly heat. This rash is very itchy and prickly, like small blisters or bumps.
Allergic Reactions

Hives, welts, body redness. Source: Allergy and Anaphylaxis Australia
Allergic reactions can manifest as skin rashes, such as eczema, contact dermatitis, and hives. These reddish, itchy, and inflamed rashes can be due to underlying viral illness or airborne allergens, food allergens, medications, contact with irritants, or insect bites.
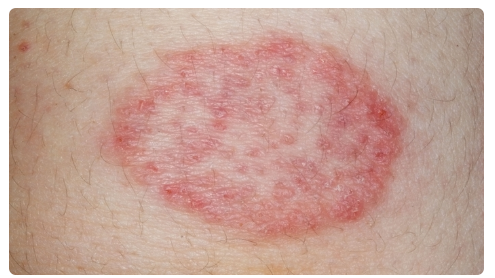
Eczema and Psoriasis

Adult eczema. Source: Eczema Support Australia
Skin rashes due to eczema are dry and itchy, while rashes in psoriasis are thick, raised, and scaly, which may affect the eyes, joints, and nails. Eczema is always itchy, reddish, and inflamed. Eczema rashes may also develop small bumps and blisters. Psoriasis and eczema can look similar but it is usually simple for a dermatologist to distinguish between the two.
Fungal Infections
Ringworm. Source: Health Direct
A fungal rash is red, swollen, or bumpy and often occurs on the nails, skin, mouth, or throat. One of the most common is the ringworm, a rash that appears circular with a clear centre and feels very itchy. Meanwhile, yeast infections cause bright red, itchy rashes along the skin folds and breasts.
Viral Rashes
Rashes due to a viral infection can vary depending on the specific virus. Skin rashes are the most prominent symptoms of a viral infection, often appearing as pink or reddish spots, flat or raised, and may form blisters or welts.
Rashes are accompanied by fever, sore throat, cough, fatigue, and headaches. Some of the most common viruses that cause rashes include chickenpox, measles, rubella, mononucleosis, and hand, foot, and mouth disease. Some cases of COVID-19 also appear with a rash.
Signs Your Rash Might Be Serious
Do not ignore skin rashes because they might indicate something serious. Consult your GP or a dermatologist for the following:
Accompanied by fever or flu-like symptoms
A rash that comes with a fever (low to high-grade fever) or flu-like symptoms (colds, cough, body aches, headaches, etc.) could be a sign of an infection. Your GP may need to run some tests to check for an infection and start you on antibiotics.
Painful, blistering or rapidly spreading rash

Painful shingles blisters. Source: Healthline
Rashes that are painful (when you press it or nearby skin) and with blisters or small pockets of fluid-filled skin should never be overlooked. Also, a rash that won’t go away or rapidly spreads across different parts of the body may indicate an acute infection or inflammation.
Skin cracking or oozing pus
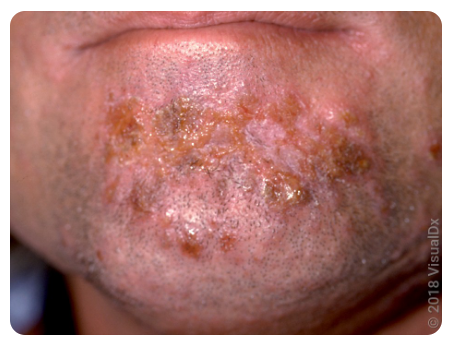
Impetigo on the face. Source: GoodRx
Rashes accompanied by skin cracking with pus oozing from the rash could be signs of a bacterial infection such as folliculitis or impetigo. In folliculitis, skin rashes are itchy and pus-filled around hair follicles. Impetigo is contagious and comes with pus-filled blisters on the face, arms, or legs.
Purple or bruised appearance
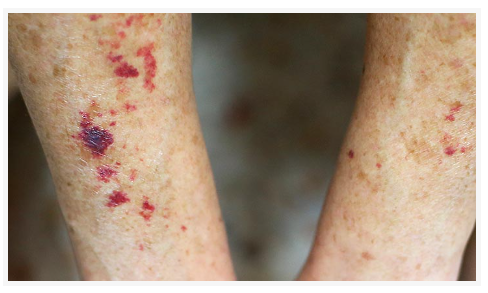
Reddish to purplish, flat rashes called purpura. Source: Cleveland Clinic
A skin rash with a purplish or bruised appearance is called purpura. These appear as small, flat spots due to bleeding underneath the skin caused by infections, blood disorders, medications, and other underlying medical conditions.
Rash with swelling or difficulty breathing
Allergy rashes can cause throat swelling and difficulty breathing. This is a dangerous situation, and patients must be rushed to the emergency department for immediate treatment. Usually, doctors administer anti-allergy medication to provide immediate relief.
If your skin rash does not improve after a week, even with medication, visit your dermatologist or GP right away. Rashes involving immunocompromised individuals require the guidance of a dermatologist.
When Should You Consult Dr Refresh
1. If unsure about the cause, individuals
Suppose you develop a rash but can’t pinpoint why; Dr Ritu will assess your medical history and help you discover the reason behind your reaction (food, medicines, contact with irritants, stress, changes in temperature, etc.). They will also suggest ways to avoid these allergens and how to manage flare-ups.
2. If the rash is recurring or chronic
Rashes that appear on and off for a week or more should be seen by a dermatologist immediately. Dr Ritu will recommend strategies to help you manage skin rashes and may prescribe medications to control them.
3. If the rash affects the face or genitals
Rashes on sensitive areas such as the face and genitals may be due to fungal infections and may need special care. Dr Ritu will prescribe antifungal treatments and medications to control itching and irritation.
4. If you’ve tried multiple treatments without success
If your rashes remain after trying different treatments, Dr Ritu can further assess your condition and may refer you for patch testing or to an immunologist if need be.
5. If it impacts sleep or daily life
Rashes can be very itchy and uncomfortable, affecting everyday life. If your rashes impact sleep and your everyday routines, Dr Ritu can prescribe medications to deal with the inflammation so you can work, sleep, or do everything as your body recovers.
How Dermatologists Diagnose and Treat Serious Rashes
1. Skin swabs, biopsy, allergy patch tests
Dr Ritu can assess serious rashes by close inspection, taking samples, and checking skin under a microscope. She can take samples of the skin, pus, secretions, etc., and send them to the lab for analysis.
2. Prescription topical cream and oral medications
After closely analysing your condition, we will prescribe topical antibiotics and medications to ease inflammation, itching, and redness. Depending on your condition, they may also give you oral medications such as antibiotics, steroids, and antihistamines to help control symptoms and help you feel more comfortable.
3. Personalised skincare plan
Every patient and every skin rash is unique. Dr Ritu will provide a personalised skin care management plan that will work with your routines, needs, and goals.
For instance, if you work in an office and commute daily, you need a skincare plan to manage your condition despite sweating and exposure to everyday pollutants and temperature extremes.
4. Ongoing care for chronic rashes
Chronic skin rashes require ongoing care, which includes avoiding triggers, following a careful skin care regimen, and following a healthy lifestyle. Dr Ritu will advise you on chronic care strategies and schedule follow-ups accordingly.
Preventing Future Flare-Ups
Most skin rashes heal on their own, but flare-ups are still possible. Avoid these by following these techniques:
1. Avoid triggers (fragrances, heat, fabrics)
Avoid wearing fragrances or using products with strong scents, as these can cause flare-ups or aggravate your rashes. Avoid extreme heat by keeping your skin cool and staying indoors whenever it’s too hot outdoors. Wear light fabrics, and avoid clothing made from polyester, nylon, and acrylic from natural fibres such as wool and rayon.
2. Moisturise daily
Apply fragrance-free skin moisturisers or lotions/creams to keep skin well moisturised. Apply moisturiser immediately after a bath to lock in moisture effectively.
3. Wear sunscreen
Wear sunscreen to protect against further damage, even with skin rashes. Sunscreen prevents sunburn and can help manage eczema and rosacea, which may worsen with sun exposure.
FAQs
1. Is every rash a sign of an allergy?
Not every rash is a sign of an allergy. Some skin rashes may be due to viral or bacterial infections, fungal infections, reactions to medications, or exposure to chemicals. It’s important to consult a dermatologist to check your skin rash and get the right treatment.
2. How long should I wait before seeing a doctor?
If your skin rash does not disappear after a few days or after taking over-the-counter medications, you should visit your GP. Your doctor will recommend that you consult a dermatologist for chronic skin rashes and rashes that do not heal on their own.
3. What does an infected rash look like?
An infected rash is red and painful and may have blisters or pus coming out. The appearance of an infected rash will depend on the cause. If you suspect that your rash is infected, consult your GP at once.
4. Can stress cause a skin rash?
Stress or extreme anxiety can weaken the immune system, which can cause physical symptoms, one of which is rashes. Stress exacerbates all skin conditions therefore reducing stress helps with all dermatological conditions.
5. Will my rash go away on its own?
Some rashes go away without medical intervention. However, some may need the help of a dermatologist for a thorough assessment and appropriate treatment. Rashes that do not go away after a week and after taking over-the-counter medications may require specialised treatment and care.